Margo Cohen (M.D. 1964) chronicles “an almost complete lack of humanity” during her husband’s cancer journey.
Author |

The whole thing didn't start with routine, preventive care.
When Margo Panush Cohen sat next to her husband, Perry, in the office of a urologic surgeon, both Cohen and the surgeon were shocked to discover that Perry's urologist had not performed a rectal exam in five years.
It was one of many missteps that Cohen (M.D. 1964) describes in Twilight Request, a 2019 book chronicling the two years between Perry's diagnosis of and death from prostate cancer under the care of preeminent doctors at what she calls Famous Cancer Hospital (not U-M).
"When my patients died, I was invited to their funerals," says Cohen, a retired endocrinologist. "But in my husband's case, I witnessed an almost complete lack of humanity."
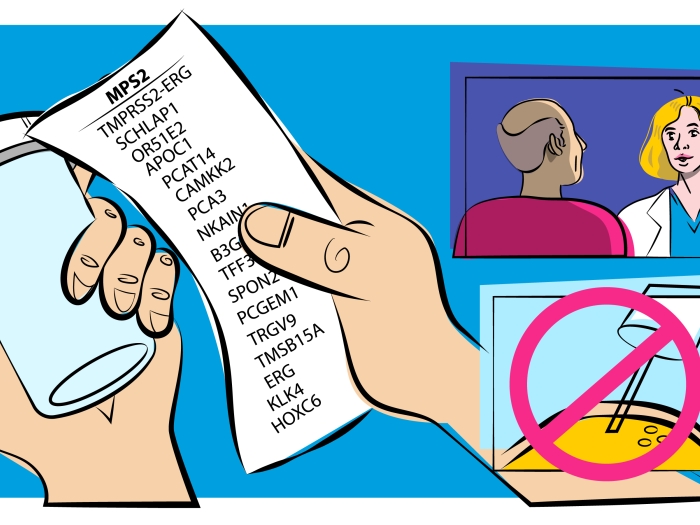
An elevated prostate-specific antigen (PSA) level first alerted Perry's urologist that something was wrong, although the Cohens' subsequent review of his records confirmed the lack of recent rectal exams and revealed that the urologist had noted but not further investigated a hard nodule that doubled in size in the year between the last rectal exams.
Thus began the Cohens' journey through a confusing and frustrating medical system that was no easier to navigate because of Margo's medical degree. Instead, she argues that her status as a doctor may have made the journey more difficult — to the point where she stopped attending Perry's appointments because his oncologist was so antagonistic.
When surgery didn't curb the spread of Perry's cancer, he came under the care of an oncologist at Famous Cancer Hospital. Of the three referrals from the surgeon, the Cohens chose this oncologist because Margo was impressed with the physician's publications and liked that she was a woman. But from the first meeting, the relationship felt off. "Anything I said was met with total disdain. She didn't like that I asked informed questions. It felt like she was patting me on the hand and sending me to the corner as she established the hierarchy," Cohen says.
In addition, Cohen says, the oncologist did not clearly convey information, misrepresented conversations in her records, and repeatedly talked down to the couple. "She practiced operation ostrich," Cohen writes in Twilight Request. "Unable to abide a truth she found disagreeable, she simply denied it."
Despite their frustrations with the oncologist, Cohen and her husband kept the faith that guides so many people under a physician's care: They believed that this hospital was Perry's best shot. Cohen says this reputation-based faith perpetuates a cycle that converts a medical team's confidence into arrogance. "They think they're God because they have a reputation for being excellent. As a result, they cultivate a sense of dependency among their patients who follow the absolutism of the voice from on high."
As a graduate of one of the country's top medical schools, Cohen understands the pitfall. She recalls early in her career feeling superior to local doctors because "as part of the University of Michigan, we were the smartest out there. Eventually you get over that if you're a mature individual. Repeatedly during my husband's treatment, though, we encountered doctors who didn't."
She also stresses that the problem is not unique to the hospital where her husband was treated. Cohen's sister died from cancer following a misread pathology report and the absence of a pelvic exam that likely would have revealed the mass that killed her. Her brother-in-law died from colon cancer after his physician failed to take a history that would have revealed his father died of the same disease.
"Many health systems have become haughty enclaves, and if one doesn't belong to the tight circle, they don't count," Cohen says. "They reinforce each other's credentials in part for self-preservation when patients die — that what happened can't be your fault because you are at the top of your game."
Can medical schools teach students to toe the line between confidence and arrogance? Cohen says it's a tough nut to crack. She stresses that while she didn't have formal coursework in patient relations as a medical student, she still became a humanistic doctor. "You either evolve in the right way or in the wrong way, and a big part of that depends on the milieu in which you practice."
Cohen was inspired to be a doctor by her immigrant father, who instilled in her the notion that medicine was the noblest profession. In addition to practicing as an endocrinologist, Cohen was a prolific researcher who earned a doctorate in biochemistry and is an emeritus member of the American Society for Clinical Investigation. She also was president and chief scientific officer of Glycadia, a company that she founded to develop diagnostic and therapeutic products for diabetes and its complications.
Regarding the cancer care that Perry received, she says, "I was mad at the behavior, the treatment, and the modus operandi, and sad that my husband died, but absolutely I'm still proud to be a doctor. I started out believing it was the greatest profession and still think it's a noble endeavor.
"But I encourage students and doctors to not lose sight of the milk of human kindness. There are huge advances in medicine, and there will be more. To be a good doctor, you have to appreciate the tools that are available, but if you can't foster a humane relationship, you might as well close up shop."