A multidisciplinary University of Michigan team has developed a device to quickly assess the immune response in pediatric patients admitted to the intensive care unit.
In most cases of injury or illness, the body will initiate the normal inflammatory immune response that allows the immune system to fight infectious agents and powers the body to start repairing damaged tissues. In up to 80 percent of patients admitted to a pediatric intensive care unit, that response becomes dysregulated, the effects of which can be quick and dangerous.
"It's important for us to know how a child's immune system is behaving in a situation like this," says Timothy Cornell, M.D. (Fellowship 2007), an associate professor of pediatrics and pediatric critical care medicine at U-M's C.S. Mott Children's Hospital and a member of the team that developed the device.
The current standard is a test measuring inflammatory proteins in the blood that can take hours to days, depending on a hospital's resources. Further, the tests require 2 to 5 milliliters, or about one teaspoon of blood. Drawing that amount of blood routinely from a sick child can be a challenge, the team says.
Cornell and his U-M colleagues, including College of Engineering faculty members Jianping Fu, Ph.D., and Katsuo Kurabayashi, Ph.D., wanted a better solution. The group's microfluidic device uses a miniscule amount of blood — 5 microliters — to provide test results in 30 minutes.
"Today, making decisions about a child's care relative to the immune response underway in his body is like standing in the middle of a teeter totter, trying to keep it balanced while blindfolded," Cornell says. "You have to guess whether you should move a little to the left or the right. With this new test, it's like you have taken the blindfold off."
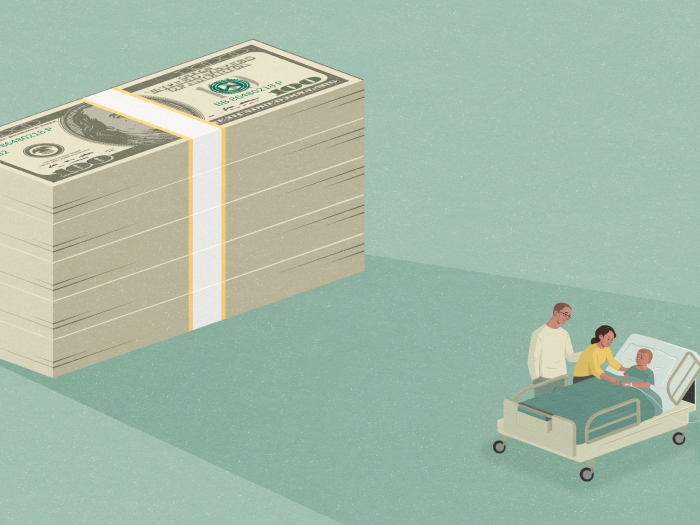
Although the new device is still in the research phase, the FDA's Compassionate Use program allowed its use in a recent pediatric cancer patient case. An oncologist was able to use information provided by the test to support adjustments to a patient's treatment and immune therapy. The patient's condition rapidly improved because of the therapy, and she was eventually discharged home.
The technology brings immune response management into a new era of precision medicine, allowing doctors to treat a patient based on his or her individual situation versus applying a standard protocol universally.
This test will help us see who's at higher risk for … sepsis and which patients may need more aggressive inflammatory modulating therapies. —Timothy Cornell, M.D.
"This test will help us see who's at higher risk for dying from sepsis and which patients may need more aggressive inflammatory modulating therapies," Cornell says. "And because this tool is faster and requires significantly less blood — we can repeat it frequently to monitor the components of the immune system we are trying to modulate to see if we've had the desired results."
Cornell and his colleagues have received funding from the Wallace H. Coulter Foundation and the Michigan Translational Research and Commercialization program to develop the processes needed to move the device from the research lab into clinical trials. They have formed a company around the new device, PreDxion Bio, to build sustainable manufacturing processes that will further expand the application of the device. Their business focus is on creating relationships with manufacturers that can help them scale production up from four to 400 devices a day.
The team expects to have a clinical trial at a handful of centers by early 2017, and hopes to expand to a large clinical trial within the next few years. Cornell says, "Five to 10 years from now, the PreDxion test could be every bit as much a standard part of an ICU doctor's arsenal as fluids, blood pressure medicines and antibiotics."