Professional musicians are athletes. That’s not just a metaphor — at least not for the speech pathologists, physical therapists, occupational therapists, laryngologists, vocal coaches, and other providers who care for them at Michigan Medicine.
Author |
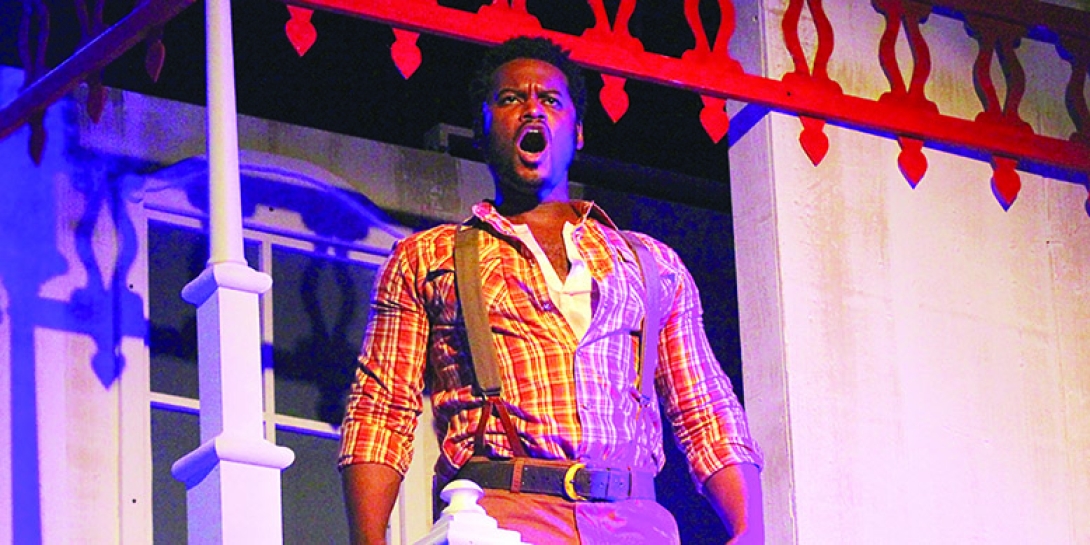
John Sloan was a musical theater major at U-M (B.F.A. 2005) and spent several years touring with the Broadway production of The Lion King. He's a singer. He's an actor. And he's a "mover." He won't call himself a dancer, because he didn't do classical dance training.
"Movers are better dancers than 95% of the world," says Sloan. "If you're out on Friday night at the club, you're like, 'He can dance pretty well.' But no, not compared to people I work with."
Still, Sloan was in the ensemble for The Lion King, which meant performing hyper-physical parts, such as a wildebeest in the stampede scene. Even if you've never seen the Broadway musical or the animated movie, you can probably guess the propulsive movement, speed, and precision needed to recreate a stampede on stage. It's an incredibly physical job that involves running, jumping, and doing explosive moves, all while singing beautifully and acting convincingly. And holding a 20-pound shield.
Musician athletes like Sloan perform eight shows a week, plus rehearsals. And when patrons are paying top dollar for Broadway-quality shows, there's very little room for error.
The Musical Theater Athlete
In April 2015, Sloan was making an entrance on stage that he had made thousands of times before. He had been touring for six years at that point, and he knew what he was doing. Just before his entrance, he was chatting with a friend. "When I went to pivot and push off, I heard and felt a pop."
It was the opening of Act II. The song was "One by One." For his entrance, he had to run through the theater, past audience members, and up onto stage. "We were in Cincinnati, and the house in Cincinnati had stairs," he recalls. "I had to time out my steps on these stairs. They want you running, flying, running down the aisle up on stage with a lot of energy.
"I get two or three steps in, and I can't feel anything below my knee."
Sloan had torn a calf muscle, and it took about three months of therapy and training with Kristen Schuyten, PT, DPT, a physical therapist on the Michigan Medicine MedSport team, to get him back on stage. "Because she had a dance background, she understood what I needed to do," says Sloan.
It's that background that helps Schuyten treat not only professionals such as Sloan, but also students. "Musical theater majors have to do everything," says Schuyten. "Their voices are instruments, and they have to dance, act, block, learn fighting styles. There's so much possibility for injury."
That's why Schuyten has partnered with Lexie Muir-Pappas, OTR/L, a certified hand therapist who specializes in treating performing artists in the occupational therapy division of the Department of Rehabilitation Therapies, to screen incoming students in the School of Music, Theatre and Dance. The two therapists look for posture problems, nerve issues, and anything that might lead to an injury down the road. Then they create individualized exercise plans for the students and report any overall trends to faculty.
"We have so much available for the athletic students," says Schuyten. "We'd like to offer as much as possible to the performing arts students [as well]. Their academic standing is dependent on their ability to move, perform, and do so freely."
The Wildebeest Learns to Walk Again
About a week into Sloan's return, he was on stage as a wildebeest in the stampede scene when he "felt a little bit of a pop." After all of his training and therapy with Schuyten, he wasn't too worried. He kept going, but then felt more pops. "I was like, 'Oh no.' I tried to keep dancing, but I didn't have the stability, the explosion, nothing." He walked off stage on what turned out to be a torn ACL and torn meniscus. He had also shattered the cartilage on his femur. And his surgeon at U-M discovered a microfracture during surgery to repair the ACL.
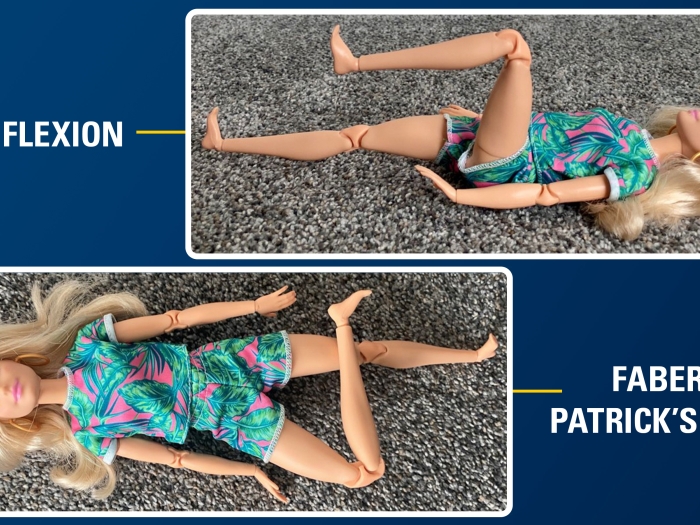
This time, it took him much longer to recover. "Kristen taught me how to walk again," says Sloan. In addition to leg presses and hamstring curls, they also addressed fine motor skills, working through ankle mobility and the articulation needed for full pointing and flexing of the foot, getting his movements as smooth as possible.
But he wasn't done with physical therapy when he regained those basic skills. Schuyten knew Sloan would need to be able to dance again, not just walk. "Kristen put me at a ballet barre, looking at my pliés to see where I'm putting my weight." Eventually, he graduated to training with a medicine ball, holding it in front of him like his prop shield while doing split leaps and jumps. He also spent time singing on a treadmill to regain his performance endurance.
"When I got frustrated when something wasn't working the way I wanted it to work, I didn't have to explain something to [Kristen]," says Sloan. "She understood what I was trying to do and how important that was to me." In other words, Schuyten treated Sloan like the elite musician athlete that he is.
After surgery and about a year and a half of therapy, Sloan was able to get back on stage.
The Percussionist Athlete

It's not just musical theater folks who are pushing their bodies to the limits for performance. Instrumentalists do as well.
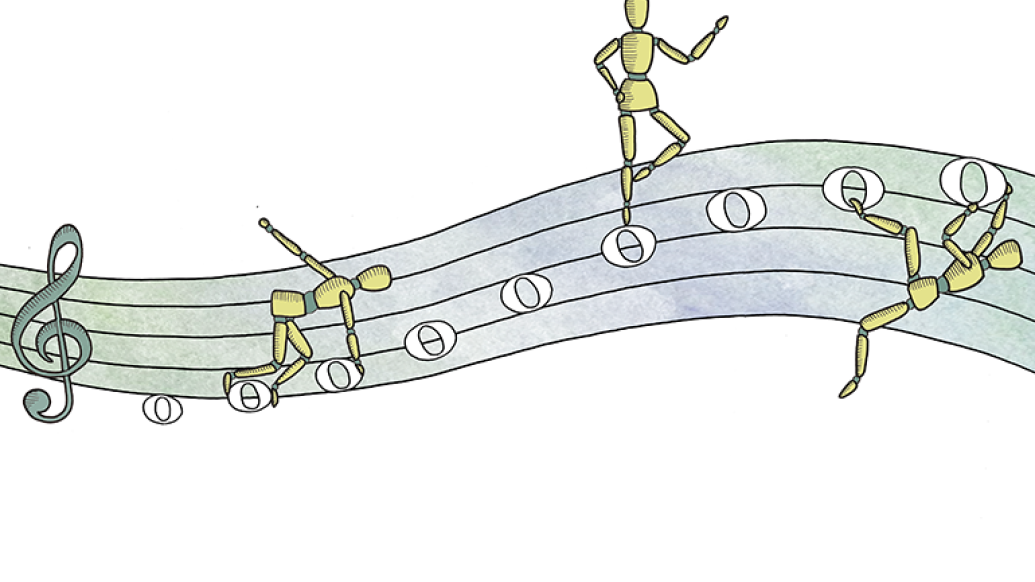
Jonathan Smith, DMA, a percussionist with the Toledo Symphony and percussion program manager at the U-M School of Music, Theatre and Dance, found his physicality tested when he was asked to perform percussion as a substitute for the Broadway production of Aladdin. He had also been working on his musical arts doctorate, which involved an expansive solo recital using big setups.
"Percussion is probably the most physical [instrument]," says Smith. In addition to the physicality of playing, percussionists also assemble their setups, which can be made up of many different instruments, including large, heavy drums.
"The Aladdin setup in New York City is built on five stations, and I'm literally running around to each station of instruments," he says. "The show is two and a half hours. Five stations: timpani, keyboard, world percussion, metal effects, and then a vibraphone concert bass drum station. They're all in this area that's maybe 10 feet by 10 feet. It's just filled with instruments."
Because of the premium on space in New York City, "there's a lot of stacked instruments," says Smith. He would be playing bongos at chest height for 10 minutes and then reach above the vibraphone to hit something. "There's a lot of movement involved. You're playing timpani and you've got a hot second to run to world percussion section, but you have to move to get to the next spot. Every show is difficult, and you can't really mess up. It's not really an option."
In addition to using sticks and mallets, he also played the world percussion with his hands. "That's probably another reason why I ended up coming to physical therapy."
Shoulder and neck pain ultimately brought him to Schuyten. One of the things that has been important for Smith's performance health is maintaining good posture while driving. It sounds simple, but all of the muscles in his upper body and torso that he needs for performance can become fatigued with his frequent trips from Ann Arbor to Toledo. He's also the cymbal player in the symphony, so he holds 20-pound plates out in front of him for a long time.
He also needed help strengthening some smaller muscles. He already knew he had a physical job, and he maintains his stamina by doing cardiovascular workouts and weightlifting. But Schuyten had him lifting a whole new kind of weight: a soup can.
"We did exercises to strengthen the little, tiny muscles," says Smith. "I'm like, 'Is this working?' But it did."
The Cellist Athlete
As an occupational therapist, Muir-Pappas' bread and butter is the little, tiny muscles. In addition to the screenings they do for incoming students, Muir-Pappas and Schuyten also host monthly open clinics, where students and faculty can drop in to get advice. Muir-Pappas looks at the musicians' posture and positioning on instruments as well as assessing how they are performing daily tasks outside of music. It was at one of these clinics that Muir-Pappas met cello student Cecelia Sha (B.A. 2018, M.A. 2020).
"I told her that when I was playing for a long time, my arm would get tired," Sha recalls. Her left ring and pinky fingers would feel especially fatigued, sometimes making her forearm feel weak. At the clinic, Muir-Pappas discovered some popping in the ulnar nerve of the elbow. It turned out that Sha had cubital tunnel syndrome. While she was in occupational therapy, she also started developing thumb pain in her right hand, which holds the bow.
"At first, therapy was a lot of 'spa treatments,'" like ultrasound massage and putting her hand in warm wax, says Sha. Then they worked out with Silly Putty to develop Sha's grip strength and also used a flexible foam bar for some exercises. Muir-Pappas also taught Sha how to tape her thumb as well as her ulnar nerve.
Sha doesn't play as much as she did as an undergraduate. She moved back to New York City during the pandemic to help out at her family's business, but she is still doing cello side gigs. Mostly weddings, she says. And she's retained a lot of what she learned from Muir-Pappas. She still works on properly using the tiny muscles in her outer thumb (as opposed to the inner pad that was originally getting overworked) and does taping as well.
Musicians "need to do a cardio warmup, elevate their heartrate for five to 10 minutes before playing, emphasize that they're athletes," says Muir-Pappas. She tells students, "Train for performances like you're a marathon runner."
When You Need Your Legs for Singing
"If you want to screw up a baseball player, right before he goes up to bat, ask him, 'How do you swing?'" says Alexandria Strother, who double majored in voice and engineering at U-M. Although she's not a baseball player, she says the saying stuck with her because the same is true for stage performers. "As a singing performer, your goal is to be in the moment; it's not to be thinking about the mechanics."
That's why she knew she needed physical therapy with Schuyten when she injured her leg as an undergrad. "Not just, 'OK, well, I hurt my leg, I just need to be able to walk down the street,'" she says. "But I needed to be able to get back on stage. I needed to be confident in heels, confident twisting and turning and not worrying about it."
Although she ended up giving her senior recital on crutches while she was still recovering, Strother did eventually get back to performing in heels.
"Kristen may have gotten kicked in the face by me once," Strother recalls with chagrin. "At the end of sessions, she would have me lie on my stomach, and she would push down on my leg to help me get that range of motion back." It was a painful exercise, so Schuyten would cue up a funny YouTube video to show Strother as a reward at the end of their session.
One time, while pressing down on Strother's leg, Schuyten lost her grip. "All your body wants to do is stop the pain," says Strother. "So I extended the leg and wacked her across the face. We were done with that exercise for the day," she says with a laugh.
Strother and Schuyten are now friends, and Strother even messaged Schuyten when she needed help finding a physical therapist in Chicago. "That was a really nice experience I had at MedSport," she says. "There was definitely a feeling of care beyond the mechanical problem, beyond insurance and filling a spot on the schedule."
The Vocal Athlete
About eight months after Sloan's long recovery from his torn ACL and related injuries, he noticed something was off with his voice. "The voice is a muscle," says Sloan. "One thing that opera does a lot better than Broadway is taking care of and prizing vocal health. Doing that much singing [for eight shows a week] is going to wear anybody down."
"All high-level voice users are at increased risk for sustaining vocal injury," says Marci Rosenberg, M.S., a speech language pathologist and clinical singing voice specialist at the U-M Vocal Health Center. "Just like a quarterback is at higher risk for sustaining injury, so are singers." Rosenberg says lesions and nodular swelling are common injuries for vocal athletes, however there are numerous scenarios that will bring a professional voice user into the clinic. "Sometimes we just see them because they have an upper respiratory infection that is untimely when they're in a show. The Vocal Health Center was created for these exact kinds of scenarios. Once they are evaluated by a laryngologist, my role as a speech language pathologist is to help them troubleshoot safely getting through a performance."
When Sloan left The Lion King tour in 2017, his voice felt raw. He thought he would need a couple of weeks rest, followed by a couple of weeks of training, to get his voice ready for two vocally demanding roles in Ragtime and Rent. For Sloan, these were the roles of a lifetime. But when he began warming his voice back up after resting for two weeks, "it just wasn't happening," he says. That's when he went to the Vocal Health Center at Michigan Medicine.
Unique, Three-Part Care for Vocalists
When Norman D. Hogikyan, M.D., F.A.C.S., laryngologist and professor and associate chair of otolaryngology-head and neck surgery, came to U-M in 1995 and founded the Vocal Health Center, he wanted to serve patients with voice disorders, in particular vocal athletes. That includes "singers, actors, teachers, preachers, courtroom attorneys, radio announcers — anyone who uses their voice publicly for a living," says Rosenberg.
Part of what drew Hogikyan to Michigan Medicine was its unparalleled collaboration. Here, he was not only able to collaborate with other medical disciplines but also with the voice department at the U-M School of Music, Theatre and Dance.
"I wanted to create a multidisciplinary clinic [at the Vocal Health Center] for occupational and professional voice users," he says. In 1996, they opened the clinic. "The three disciplines that I brought together in that were laryngology (voice doctor), speech pathology, and vocal arts."
At the time, adding an artistic component to evaluation and treatment "was very novel," says Hogikyan. But he knew, for vocal athletes, that innovation would be a key component to caring for the whole person. "This team approach proved to be incredibly synergistic with respect to quality of care, and for finding great purpose in our shared work. I am blessed with outstanding colleagues today and have been from the very beginning."
For Sloan, that extra attention has been an invaluable part of his care at the Vocal Health Center. "What to me is the through line of working with U-M is this understanding of the importance of my craft. Dr. Hogikyan, Marci, and everyone in the office — Maureen at the front desk — understands this is how I make a living."
After his initial consultation with the Vocal Health Center team, Sloan needed surgery for steroid injections in his vocal cords, medication and dietary changes to manage acid reflux, and extensive singing voice rehabilitation with Rosenberg.
How Do You Measure the Importance of a Voice?
"What the impact of a voice disorder means to an individual is subjective," says Hogikyan. "But it's important to try to measure that, because it helps you to connect with and understand each patient as a person, and it can guide the nature and intensity of treatment." That's why Hogikyan and his colleagues developed a tool to measure voice-related quality of life (V-RQOL).
They published the results of a clinical research study showing the validity of the tool in 1999. Since then, the 10-item V-RQOL Measure has been translated into more than a dozen languages and has become a standard tool for voice assessment.
"Our voice is central to who we are," says Freda Herseth, the Arthur F. Thurnau Professor of Voice at U-M and a voice training specialist at the Vocal Health Center. "It's like the fingerprint of our soul. How we're feeling comes through the voice. If we're tired, it's in the voice. If we're excited, it's in the voice."
In the back of his mind, Sloan knew he would age out of doing incredibly physical musical theater performances, but he thought he would always have his voice. "I've had my voice since I was born," he says. "When you take away someone's instrument from which they communicate, not just what they use for their art, but how they express themselves, how they talk through their fears, joys, apprehensions — the emotional weight on that is huge."
There were sessions when he and Rosenberg spent a large part of their time talking through his worries that he might not be able to get back to singing.
"It might be a physical rehabilitation, but it requires an emotional and mental component as well," says Sloan. "I feel for colleagues and friends of mine who've had to go through similar processes without that type of support, [which] is not always seen and regarded as necessary.
"When you're dealing with artists, our job is to process emotion in public. We process pain, joy, fear, and sadness for public consumption. We build a muscle around the accessibility to those emotions."
While his physical and emotional muscles were recovering, Sloan had to give up those roles in Ragtime and Rent, but he did eventually make it back to performing. It meant relearning a whole new way of singing. Sloan learned that his classical and traditional operatic training was not the best suited to the "belt technique" that is a hallmark of Broadway musicals. With exercises such as trying to sing through a straw or practicing different laryngeal positions, Sloan learned new techniques from Rosenberg that would protect his voice better during contemporary musical performances.
"The benefit I had from working with Kristen and Marci and really the whole team … was the way they treated me like a person, the way they regarded and respected my art."
How to Avoid Injury
Experts give us their best advice for how to stay healthy — whether you make music or not.
1. Don't smoke or vape, says Norman D. Hogikyan, M.D., F.A.C.S., laryngologist and professor and associate chair of otolaryngology-head and neck surgery. He says he sees a lot of smoking-related conditions in his patients, and "it's a complete contradiction in commitment for a singer to smoke."
2. "Think about a voice budget," says Marci Rosenberg, M.S., a speech language pathologist and clinical singing voice specialist at the U-M Vocal Health Center. "If you go to a football game and you yell and scream, you are putting a significant amount of effort and friction on the vocal folds." Hogikyan agrees: "It's never healthy to be a screamer or yeller," he says. "Use amplification when possible, if speaking over background noise or in large open spaces. It allows you to speak with conversational vocal intensity and yet reach your targeted audience."
3. "Listen to your voice when it's complaining to you," says Hogikyan. "If you have what might be a garden variety laryngitis, pull back a bit on your voice use for a while, and you'll be less prone to injury such as hemorrhage or a polyp." Rosenberg says, "Hoarseness is abnormal. It doesn't just show up for no reason. [If someone is] experiencing any decline and change in vocal quality, hoarseness for more than a few weeks that's not due to illness or infection, they need to see a laryngologist or ear, nose, and throat specialist to see what's going on."
4. "Your speaking voice and singing voice are the same thing," says Freda Herseth, the Arthur F. Thurnau Professor of Voice at U-M and a voice training specialist at the Vocal Health Center. "Learn how to speak well instead of speaking down in your throat," she says. "Pitches that are too low, monotone, or gravelly use little air and are very tiring for the voice." To find out if someone is speaking down in their throat, Herseth does the "mm-hm test." She asks a series of yes or no questions and tells the speaker to respond with "mm-hm" or "hm-mm." Those sounds are usually made at the person's natural pitch area, with adequate breath flow. She finds where their mm-hms are on the piano and then compares it to their speaking voice. "Often it will be disjointed, and one will be a third higher than the other."
5. "Be a good listener," says Herseth. "Sometimes you can give your voice a good rest when you need one."
6. "Posture, posture, posture!" says Lexie Muir-Pappas, OT, a certified hand therapist who specializes in treating performing artists in the occupational therapy division of the Department of Physical Medicine and Rehabilitation. She says posture is especially important when you're using a computer or a cell phone.
7. "My soapbox is the importance of warm up and cool down," says Kristen Schuyten, PT, DPT, a physical therapist on the Michigan Medicine MedSport team. "So many instrumentalists equate 'warmup' to performing scales, or warming up only their embouchure. The back, shoulders, neck, abdominals, and hips are all needed to help your hands and arms to manipulate your instrument. A light, whole-body warm up and stretching out after performance or after classes, those are huge steps to injury prevention." Rosenberg echoes this sentiment, emphasizing the importance of vocal warm up and cool down for vocal health.
8. "I tell [music students] they need to be buff. They need to work out," says Muir-Pappas. "People I see who are more fit coming into this are less likely to get injured."
9. "Hydrate," says Hogikyan. "Moisture is good for the voice, and dryness is bad."